
Table of Contents
ToggleTan Siak Meng Occupational Therapist
I am Simon Tan, a Malaysia-registered Occupational Therapist (MAHPC) with clinical experience since 2010.
For the past 14 years, I have focused on chronic pain management, neurorehabilitation, and upper-limb functional recovery, especially for stroke survivors and individuals with long-standing movement limitations.
My clinical approach combines anatomical assessment, neuromuscular control training, and evidence-based manual techniques such as PNF (Proprioceptive Neuromuscular Facilitation), dry needling, and trigger point therapy to restore efficient, pain-free movement.
Professional Credentials
Education
Bachelor of Science in Occupational Therapy
Kaohsiung Medical University (KMU), Taiwan
Certifications
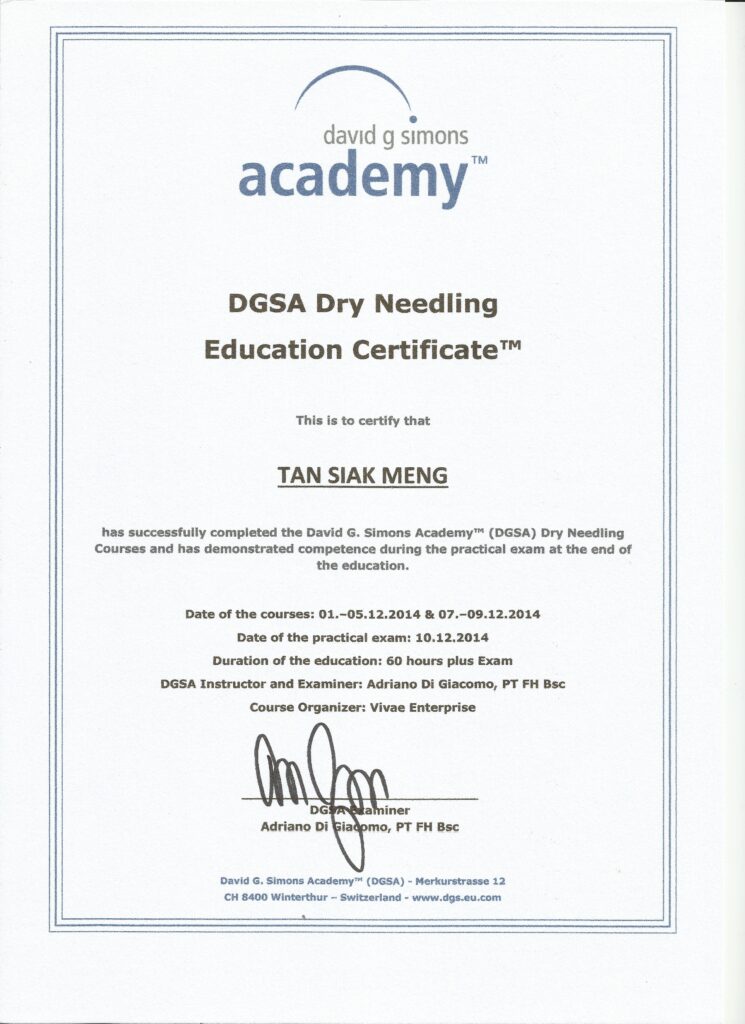
DGSA Certified Dry Needling Therapist(2014)
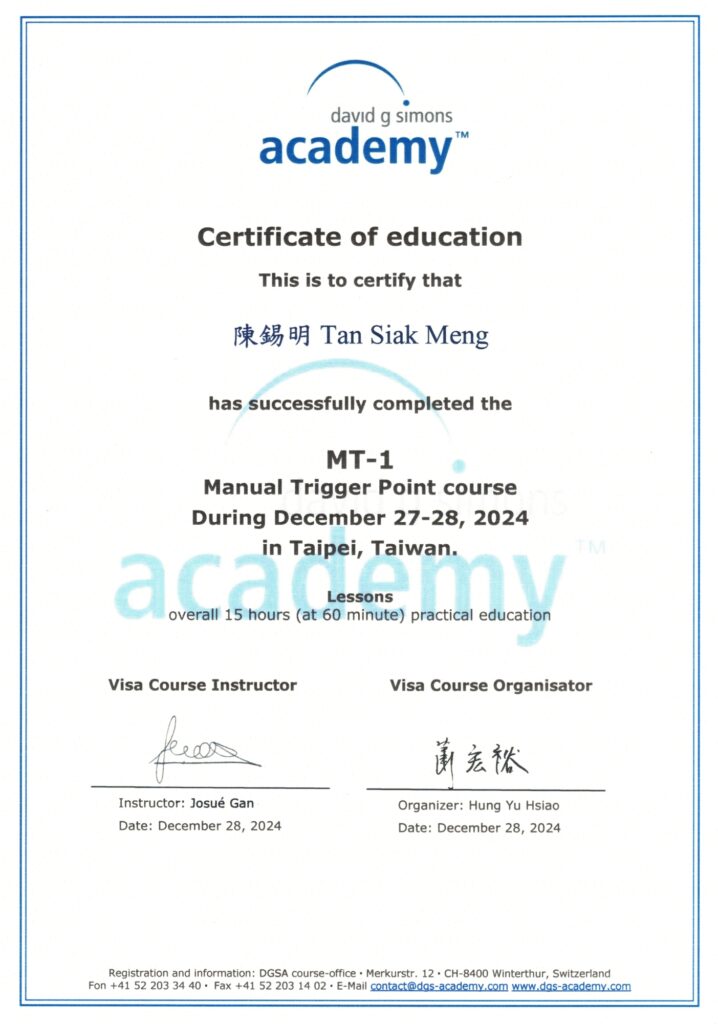
DGSA Manual Trigger Point Therapy(2024)
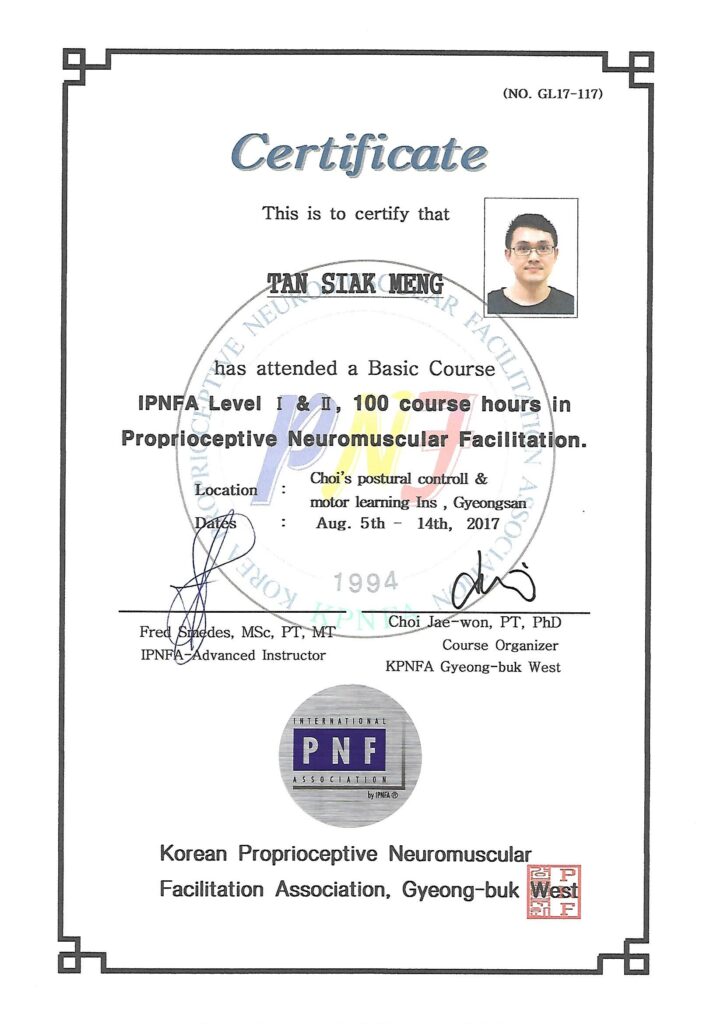
IPNFA PNF Level 1 & Level 2 Certification (2017)
BTE Functional Capacity Evaluation (2012)
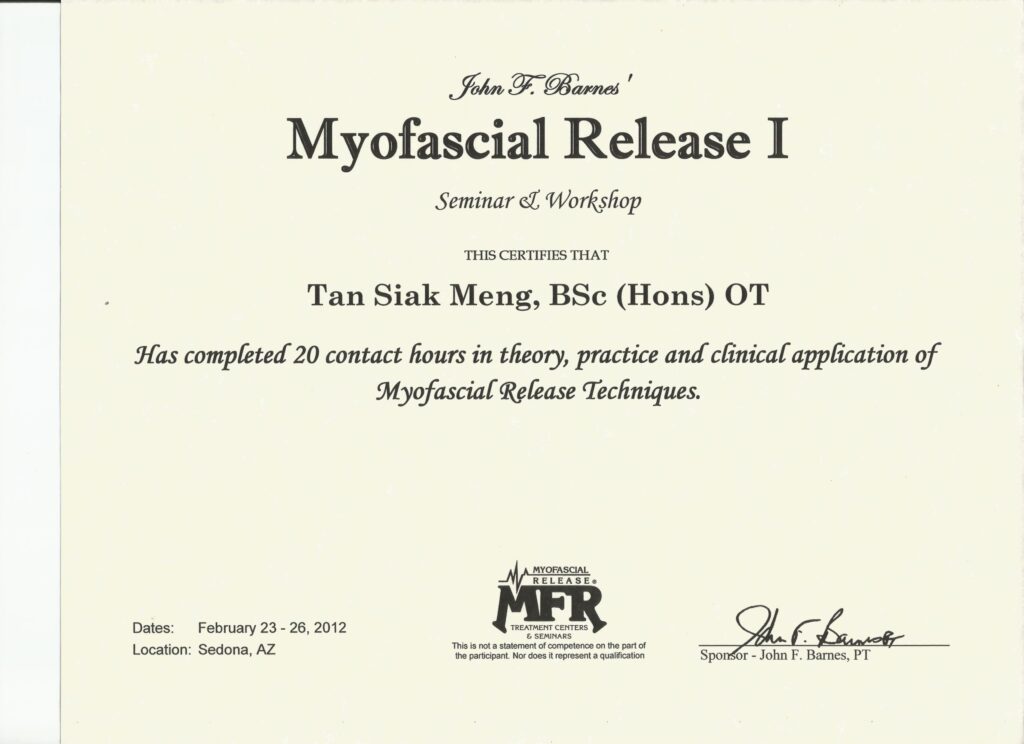
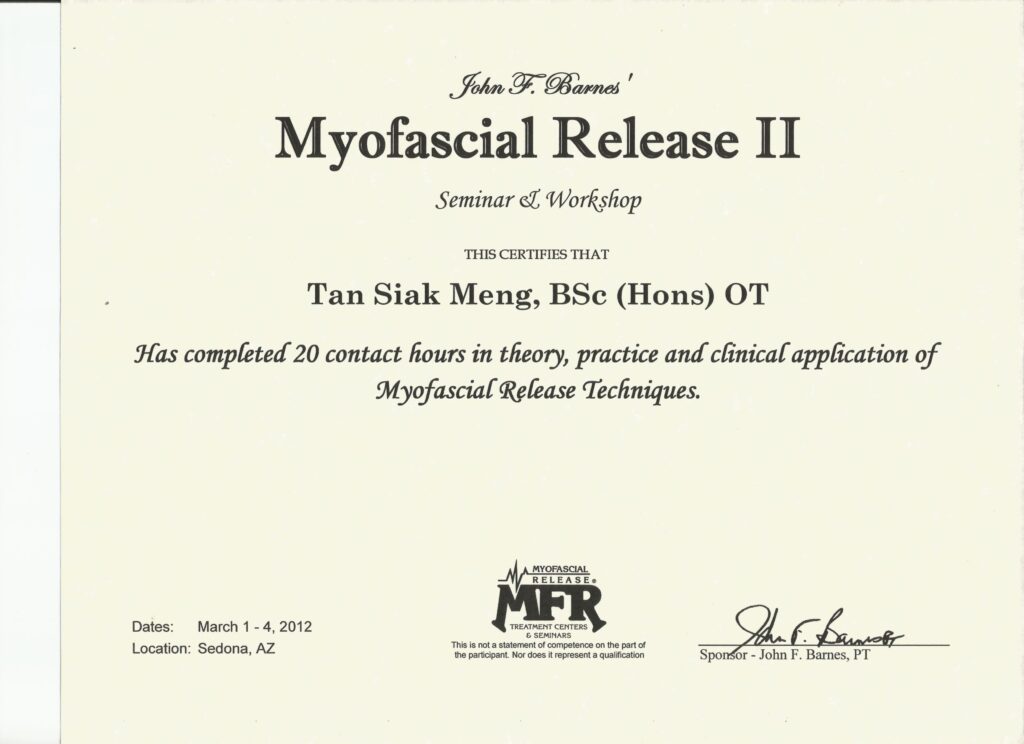
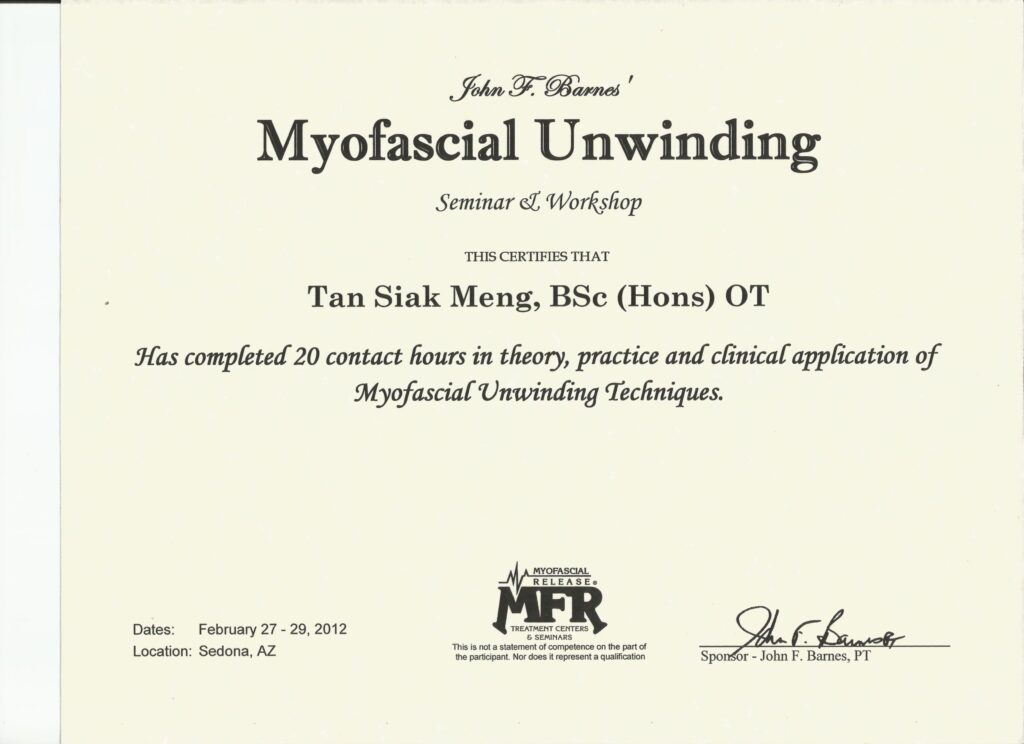
John F. Barnes Myofascial Release Therapy(2012)
WFOT & OT Malaysia Registered Member
Clinical Experience
Occupational Therapist, Sau Seng Lum Rehabilitation Centre (Work Rehabilitation Department), 2010–2017
Home-based & Freelance Occupational Therapist, 2017–2018
Founder & Senior Therapist, Integrated Rehabilitation and Wellness, 2018–Present
Clinical Philosophy
For Chronic Pain Management
Muscles, fascia, ligaments, tendons, periosteum, nerves, joints and tendon sheaths can all generate pain when they are irritated or injured. Through careful, step-by-step assessment and clinical testing, we look beyond the surface symptoms to identify the true source of your pain.
My goal in occupational therapy is more than pain relief.
Starting from your everyday posture, movement patterns and work habits, I look for the underlying drivers of your pain and gradually break the vicious cycle of pain, guarding and stiffness. By restoring active muscular control and coordinated movement, I help you return to a more independent, active and confident life — at home, at work and in the community.
For Neurological Rehab
After a stroke, the issue is not that patients “don’t want to move.”
It is that the brain temporarily loses its ability to control the affected muscles. During this phase, passive movement alone is often not sufficient to promote meaningful recovery.
The core of neurological rehabilitation is to activate weak or impaired muscles, and gradually rebuild the connection between the brain and the body.
Through proper facilitation, targeted stimulation, and task-oriented functional training, the brain can relearn how to control movement—allowing the affected limb to regain strength, coordination, and purposeful action over time.
For Cognitive Rehab
Cognitive abilities may decline due to brain injury, neurological conditions, or the natural aging process. Through a structured cognitive assessment, we identify difficulties in areas such as attention, short- and long-term memory, executive function, and spatial orientation.
Cognitive rehabilitation focuses on targeted, individualized training to strengthen these abilities. The goal is to enhance the brain’s processing capacity, improve daily functional performance, and help patients regain clearer thinking, better judgment, and greater independence in everyday life.
Areas of Expertise
Pain Management
Neck & shoulder pain
Low back pain
Sciatica
Myofascial pain syndromes
Chronic stiffness or muscle imbalance
Neurological Rehabilitation
Post-stroke upper limb recovery
Hand function rehabilitation
Motor relearning & coordination training
Tone management (spasticity / flexor synergy patterns)
Work & Functional Rehabilitation
Return-to-work programs
Movement pattern correction
Trigger point integration with functional tasks
Treatment Approach
1. Comprehensive Assessment
Posture & movement analysis
Functional task breakdown (reaching, gripping, lifting)
Joint mobility & neuromuscular control assessment
Trigger point mapping & palpation findings
2. Treatment Planning
Clear goals tailored to your occupation, lifestyle, or sport
Stage-by-stage functional progression
Pain reduction + mobility restoration + movement retraining
3. Clinical Interventions
PNF neuromuscular facilitation
Manual trigger point therapy
Dry needling (when clinically appropriate)
Joint mobility training
Task-specific functional retraining
Customised home exercise program
4. Follow-Up & Progress Review
Functional outcome tracking
Movement quality reassessment
Gradual return to daily tasks, work, or sports
Dry needling is performed only when clinically indicated, with risk–benefit explanation and patient consent.
Certifications & Professional Memberships


Clinic Information
Integrated Rehabilitation and Wellness
86G, The Earth Bukit Jalil, Kuala Lumpur
WhatsApp: 013-583 8188
Email: integrehabwellness@gmail.com
Website: https://interehab.com
